Introduction
Consult The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist guide for parents of children and teens. Understand systematic desensitization, food chaining, and nutritional rehabilitation, and learn how this complex condition is managed through a collaborative, expert therapeutic team approach.
The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist approach is essential for managing this complex eating disorder, which involves significant dietary restrictions driven by a lack of interest in food, extreme sensory-based avoidance, or a profound fear of adverse consequences (like choking or vomiting). ARFID is far more severe than typical picky eating and often results in clinically significant nutritional deficiency, dependence on nutritional supplements, or marked psychosocial impairment.
Because this disorder typically stems from deep-seated anxieties or sensory processing challenges, treatment requires advanced, systematic training, almost always as part of a collaborative team that includes a feeding therapist, a registered dietitian, and a medical doctor. The pathway to recovery involves detailed systematic desensitization, strategic food chaining, and focused nutritional rehabilitation.

1. Understanding the ARFID Profile and the Team Approach
The first step in working with The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist is recognizing that ARFID presents differently from patient to patient, necessitating a highly individualized, multi-disciplinary approach.
The Three Drivers of ARFID (Avoidant/Restrictive Food Intake Disorder)
ARFID is clinically defined by three primary behavioral presentations, which often overlap:
- Sensory Avoidance: The individual restricts intake based on extreme sensitivity to the sensory characteristics of food, such as texture, smell, or temperature. This is where systematic desensitization is most effective.
- Lack of Interest: The individual exhibits low appetite or simply forgets to eat, often showing a profound disinterest in the eating process or the social aspects of food.
- Fear of Aversive Consequences: The individual avoids certain foods or textures due to a past negative experience, such as a severe choking incident, extreme nausea, or prolonged vomiting.
Because these factors touch on mental health, physiological health, and nutrition, the most effective management of ARFID (Avoidant/Restrictive Food Intake Disorder) relies on a specialized team—not just the parent.
The Interdisciplinary ARFID Team
The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist (often a feeding therapist or licensed clinical psychologist) guides the behavioral interventions. They collaborate closely with:
- The Physician/Pediatrician: To monitor growth, vital signs, and address any physiological issues (like severe reflux or GI pain) that might be driving the fear component.
- The Registered Dietitian (RD): To conduct comprehensive nutritional assessments, nutritional rehabilitation, and ensure the diet is safe, adequate, and high-performing, even when restricted.
This coordinated, holistic approach is non-negotiable for successful treatment of ARFID (Avoidant/Restrictive Food Intake Disorder), particularly in achieving sustainable anti-aging health by preventing long-term systemic damage from malnutrition.
2. Systematic Desensitization: Addressing Fear and Sensory Avoidance
The central therapeutic tool for the sensory and fear-based drivers of ARFID is systematic desensitization. This process slowly and patiently exposes the individual to the avoided food characteristics in a completely controlled, low-anxiety environment, aiming to re-program the brain’s fear response.
Building the Fear Hierarchy
The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist first works with the patient to build a fear hierarchy, a list of food-related tasks or exposures ranked from the easiest (low-anxiety) to the hardest (high-anxiety). This list is based on the child’s specific triggers—a child with texture aversion might rank ‘touching cooked spinach’ as difficult, while a child with fear of choking might rank ‘chewing meat’ as difficult.
A typical hierarchy step might look like this:
- Tolerate the food in the room.
- Tolerate the food on the plate.
- Touch the food with a fork.
- Touch the food with one finger.
- Smell the food deeply.
- Bring the food to the lips.
- Take a small lick/kiss.
- Place the food in the mouth (and immediately spit out).
- Chew and swallow a tiny bite.
Implementing Exposure and Response Prevention
During therapy sessions, the ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist systematically guides the patient up the hierarchy, pausing at each step until the anxiety significantly decreases—the core of systematic desensitization. The therapist uses response prevention by guiding the patient through coping mechanisms instead of allowing them to flee or avoid the food. The therapist maintains a calm, highly predictable environment, using clear verbal scripts to reassure the patient they are in control and that there is no pressure to eat. This process teaches the patient that the feared food or sensation is not inherently dangerous. The success of systematic desensitization hinges on the repetition and consistency carried over into the home environment.
3. Food Chaining: Expanding the Repertoire and Addressing Nutritional Gaps
While desensitization addresses the fear, food chaining is the concrete strategy used by The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist to systematically expand the limited repertoire of accepted foods and target key nutritional gaps.
The Food Chaining Technique
Food chaining uses the sensory properties of a safe food to bridge to a new food. It leverages the child’s existing acceptance criteria (e.g., they only eat crunchy, white, salty foods) to introduce variations.
Example Chain:
- Safe Food: A specific brand of plain, salty potato chip (White, crunchy, salty).
- Step 1: Introduce a different brand of potato chip (Same: crunchy, salty; New: slight difference in taste/texture).
- Step 2: Introduce a similar food item (e.g., a corn chip or a cracker) (Same: crunchy, salty; New: different shape, grain).
- Step 3: Introduce a vegetable in a crunchy, salty form (e.g., a salted sweet potato fry that is very firm) (Same: crunchy, salty; New: color, vegetable).
The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist is constantly looking for the small differences the child can tolerate, making tiny, incremental changes to texture, flavor, temperature, or color. This method is far less threatening than introducing a completely novel food, as it respects the child’s sensory boundaries.
Prioritizing Nutrition with Food Chaining
The RD on the ARFID team uses food chaining to target specific nutritional deficits. For example, if a child is low in protein and only eats chicken nuggets (crunchy, salty), the food chain might move toward slightly less processed poultry, then baked poultry, aiming to introduce a safe, whole-protein source that can reduce reliance on highly processed foods. This targeted application of food chaining ensures that expanding the diet directly contributes to nutritional rehabilitation.
4. Nutritional Rehabilitation and Long-Term Systemic Health
The ultimate goal of The ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist approach is nutritional rehabilitation—reversing deficiencies, restoring growth, and establishing a maximally diverse diet that supports lifelong health.
Addressing Deficiencies and Faltering Growth
The RD uses the systematic desensitization and food chaining progress to adjust the child’s nutritional plan. This often involves:
- Formula Dependence: For severe cases, elemental or semi-elemental medical formulas may be necessary to guarantee 100% of nutrient needs are met. The RD guides the use of these formulas to maintain growth until enough whole foods are accepted.
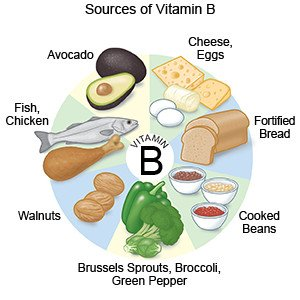
- Targeted Supplementation: Specific vitamins (B-vitamins, D) and minerals (Iron, Zinc) that are lacking due to restriction are supplemented under medical supervision to prevent conditions like anemia or bone density issues.
Sustaining Health and Anti-Aging Performance
Chronic malnutrition and the stress of ARFID put immense strain on the body, potentially impacting long-term systemic health. By focusing on nutritional rehabilitation, the ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist works to mitigate these long-term risks. Achieving a diverse, nutrient-rich diet that the child is comfortable and confident eating reduces chronic stress and systemic inflammation. This is the essence of anti-aging performance: maintaining a strong, resilient system by ensuring consistent, high-quality fuel. The success of the ARFID specialist’s intervention is measured not just by the number of foods accepted, but by the child’s return to a healthy growth curve and their reduction in food-related anxiety. For more resources on systemic health factors, including the relationship between chronic inflammation and cardiovascular wellness, consult cardiachq.com.
As an ARFID (Avoidant/Restrictive Food Intake Disorder) Specialist, what is the single most important piece of advice you give to parents struggling with the lack of interest driver of ARFID? Share your insight!