Celiac disease constipation in children is a symptom that can paradoxically present in children with celiac disease, even though the condition is more commonly associated with chronic diarrhea. This symptom is often overlooked or mistaken for routine childhood constipation, delaying the diagnosis of celiac disease. Recognizing and actively treating the constipation is a vital part of managing the disease. It’s estimated that approximately $15\%$ to $20\%$ of children with celiac disease present with constipation as their main symptom, making it a significant, though less discussed, clinical finding.
1.Why Celiac Disease Causes Constipation
To actively deal with celiac disease constipation in children, you must understand the mechanisms by which an autoimmune disease known for causing loose stools can, in fact, cause a profound “backup.”
The Damage and the Backup
- Malabsorption and Fluid Dynamics: While the small intestine is damaged, it struggles to absorb nutrients. In some children, this damage leads to an over-absorption of fluid in the large intestine. The body, deprived of water, attempts to reclaim as much as possible, resulting in dry, hard stools that are difficult to pass.
- Motility Changes: The chronic inflammation and autoimmune activity associated with celiac disease can alter the nervous system’s control over the gut, slowing down the movement (motility) of stool through the colon.
- Anemia-Related Fatigue: Iron deficiency anemia, a common finding in active celiac disease, can cause extreme fatigue and muscle weakness, including weakness in the abdominal muscles necessary for actively passing a bowel movement.
2. Active Management Post-Diagnosis: The GFD Pitfall
The most crucial step in treating celiac disease constipation in children is the strict adoption of the gluten-free diet (GFD). However, the GFD itself can, ironically, make constipation worse if not carefully managed.
The Gluten-Free Diet Trap
Many commercially available gluten-free (GF) products (like breads, cookies, and pastas) are often made with highly processed starches (tapioca, potato, corn) and are significantly lower in fiber than their whole-grain, gluten-containing counterparts.
- Low Fiber Intake: A diet high in these processed GF foods and low in naturally fibrous fruits, vegetables, beans, and GF whole grains (like quinoa and brown rice) will inevitably lead to hardening of stool and worsening celiac disease constipation in children.
- Lack of Hydration: Children who switch to the GFD might also inadvertently reduce their fluid intake, particularly if they are replacing whole foods with dense, packaged GF products.
Active Dietary Correction: Fiber and Fluid
Your active goal must be to ensure the GFD is healthy and rich in natural fiber.
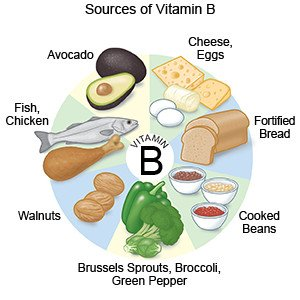
- Increase Soluble and Insoluble Fiber: Focus on naturally gluten-free foods: lentils, beans, berries, apples, pears, vegetables (broccoli, carrots), and GF whole grains. Aim for a target of fiber intake (age + 5 grams per day is a good starting point, e.g., a 7-year-old should aim for 12 grams).
- Boost Fluid Intake: Make sure your child actively drinks plenty of water throughout the day. Water is essential for making fiber effective and keeping stools soft and easy to pass.
- Limit Processed GF Items: Treat packaged GF snacks and baked goods as occasional treats, not staples.
3. Medical Interventions and Support
For severe celiac disease constipation in children, especially if it has led to fecal impaction, active medical intervention is necessary to clear the blockage and retrain the bowel.
The Clean-Out Phase
If your child is severely constipated, the doctor will likely prescribe a “clean-out” using high doses of polyethylene glycol (PEG, or Miralax) or other osmotic laxatives to physically clear the accumulated stool. This $100\%$ clearing is essential before maintenance treatment can begin.
Maintenance Therapy
Once clear, the goal shifts to keeping the stool soft and regular to prevent recurrence of celiac disease constipation in children.
- Osmotic Laxatives: PEG is often continued daily at a lower, maintenance dose for several weeks or months. It works by drawing water into the colon, keeping the stool soft. It is generally considered safe and non-habit forming.
- Stimulant Laxatives: These should be used sparingly and only under strict medical direction, as they cause the bowel muscles to contract.
- Probiotics: While not a cure, certain probiotic strains may help regulate gut motility and improve the symptoms of celiac disease constipation in children. Discuss options with your pediatric gastroenterologist.
4. Addressing Behavioral and Toilet Habits
Celiac disease constipation in children is often complicated by learned behaviors. Painful bowel movements can cause a child to actively withhold stool, creating a vicious cycle of impaction and pain.
- Scheduled Sitting: Implement a post-meal toilet sitting schedule (e.g., 5-10 minutes after breakfast and dinner). This leverages the gastrocolic reflex—the natural urge to go after eating. Encourage a relaxing, unhurried environment.
- Proper Posture: Ensure your child has a footstool (like a Squatty Potty) so their knees are above their hips. This posture relaxes the puborectalis muscle, making passage easier.
- Positive Reinforcement: Use a reward system (stickers, praise) for sitting on the toilet and successfully passing a bowel movement. Never punish or scold for accidents.
5. Checking for Persistent Non-Response
If your child’s celiac disease constipation in children does not improve despite a strict GFD, active medical maintenance, and addressing behavioral factors, you must investigate other causes.
- Accidental Gluten Exposure: The most common cause of ongoing symptoms. Even a small amount of hidden gluten can perpetuate the inflammation and motility issues. Review all sources of cross-contact.
- Co-existing Conditions: Other conditions like hypothyroidism (an underactive thyroid, which is an associated autoimmune condition) or other gut motility disorders must be actively ruled out by your doctor.
- Celiac Disease Constipation in Children can also be a presentation of functional constipation, which may require long-term behavioral therapy alongside medical treatment.
Conclusion: Consistency is Key
Successfully overcoming celiac disease constipation in children requires a $100\%$ consistent, active effort on three fronts: optimizing the fiber and hydration in the GFD, using stool-softening medication as directed by a specialist, and addressing any learned withholding behaviors. Remember that while celiac disease increases the risk, constipation is a manageable issue. With patience and a proactive approach, you can restore comfortable bowel movements and ensure your child’s quality of life improves. The risk of the most severe form of non-responsive celiac disease in children is less than $1.9\%$, emphasizing that most issues, including constipation, are highly correctable.
For further reliable guidance on children’s health issues and complex gastrointestinal care, you can consult trusted medical information sites like cardiachq.com.
Now, we want to hear from you: What active dietary change (e.g., a specific high-fiber food or drink) did you find was the most effective in helping your child finally overcome celiac disease constipation in children? Share your tip below!