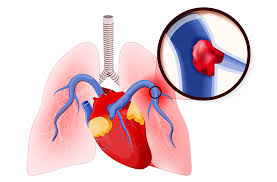
Pulmonary embolism (PE) has been synonymous with a pulmonary disorder, however, evolving data shows Pulmonary embolism (PE) as a cardiovascular emergence of types equal to or worse than cardiac arrest that keeps the cardiologists on toes. The encroachment of a blood clot on the pulmonary arteries evokes a series of events that mainly endangers the heart, especially the right ventricle. This complex PE and cardiac functional interaction is the reason why cardiologists find it as one of their most challenging tasks.
Pulmonary Embolsm
1.Pulmory Embolism: A Leading Cardiovascular Killer
- Third leading killer of cardiac deaths: After heart attack and stroke PE ranks as the second leading cause of death among people in United States with over 100,000 Americans dying each year because of PE.
- High rates of death: Close to 30 percent of the untreated cases of PE are lethal with most of them dying several hours after the development of the symptoms
- Underdiagnosed risk: A significant percentage of the sudden deaths of the heart occur on the posthumous diagnosis of PE, which identifies an issue of diagnosis
2. The Right Ventricle Under Siege
The sensation that they experience on the heart, when a PE strikes so as to cause the closing of the lungs, is as-you-go the worst:
- Overload pressure: There is actually a sudden excessive high pressure given to the pulmonary artery to fit into and the right ventricle (RV) then pumps by inducing:
- Dilation and RV hypokinesis
- atrophy of interventricular septum
- Poor filling of left ventricular and cardiac production
- Biomarkers data: the abundance of cardiac biomarkers (troponin, BNP) at the moment of strain in the RV, i.e. myocardial injuries already took place, and the outcome cannot be positive
- Electrical instability Life threatening arrhythmias (atrial fibrillation, ventricular tachycardia) frequently occurs in 50 per cent of PE patients due to hypoxia and stress resulting in electrical instabilities
Massive PE is merely a heart attack in the heart right chamber, which is highly prone to evolve into the obstructive shock in only a few minutes. Its right ventricle was not suited to such a sharp pressure overload, so to speak. The opinions of intervention Cardiologist
3.The pitfalls and duplications of pulmonary embolism
One of the masquerades of PE is another cardiac crisis:
- Chest pain misdiagnosis: a form of misdiagnosis of that chest pains cause radiates to the chest area, can possibly be due to the activity of breathing, and could be either pericarditis or ischemia
- Biomarker confusion: concentration of troponin in PE-induced RV strain is higher than PE-induced stress of acute coronary syndrome
- Confounders of the ECG: PE could appear in the form of the right axis deviation, T wave inversion, or S1Q3T3 signature, which is the same as ischemia
- Skills in echocardiography: The cardiologists are skilled in detection of RV strain pattern and are, therefore, very crucial in facilitating rapid diagnosis
4. Advanced Interventions of pulmonary embolism: The Cardiology Frontier
The PE management is the frontier of innovations, which are provided by cardiologists:
- Catheter directed thrombolysis: low doses of catheter based thrombolytic therapy and safe delivery of thrombolysis to patients without systemic effects: (ultrasound enhanced) catheter directed thrombolysis using system such as the EKOS system (7-14mg tPA versus 100mg historical systemic dose)
- Mechanical thrombectomy: Clot removal in unstable patients involves a less time-consuming procedure in which a swift removal of clots aided by a computer such as inari flow triever and Penumbra is implemented.
- PERT (Pulmonary Embolism Response Teams): These are teams of multiple disciplines that allow and make quick treatment of the patients feasible by means of rapid multidisciplinary response (structured by cardiologists).
- Innovation Impact: All these inventions have changed the way one has to handle the PE and when the risk of the death is at the said period of time which was 1-3 percent hence adding to the increase in 30 percent of the PE that will happen in case of treated improperly and 30 percent in case of treatment at the start of the treatment.
5. Long -Term Cardiac Consequences due to Pulmonary Embolism
Its cardiovascular response is far beyond the initial experience:
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH): It is seen in 2-4 individuals of every 100 individuals who survive PE, and the illness results in right heart failure that gets progressively worse
- Subclinical strain persistence: In most survivors, the much-reduced tolerance to exercise is caused by subclinical strain persistence
- Sudden occurrence of rapid atherosclerosis: PE is related to the systemic inflammation of the endothelium, which, most likely, will result in the chronic exacerbation of the cardiovascular disease
- Puts future CVD at risk: PE patients develop future CVD in form of heart failure, stroke and MI years later but at a significantly greater proportionate rate
6.Prevention of Pulmonary Embolism: A Cardiologist’s Mandate
Cardiac specialists are important in the prevention of a repeat PE:
- Anticoagulation strategy: The choice of agents (DOACs instead of warfarin) should be done following cardiovascular morbidity
- Risk factor control: Intensive treatment of obesity, high blood pressure and smoking- The CVD and PE have common risks
- IVC filters: They should be applied in limited patients who have contraindications to anticoagulation
Proactive Measures of Pulmonary Embolism: PE prophylaxis has become part of the standard care of cardiologists when attending to cardiac patients in hospital, both during and after surgery, as they understand that cardiac patients are at a higher risk of PE
Conclusion of Pulmonary Embolism: A Cardiovascular Imperative
The outcomes in pulmonary embolism become more beneficial through proper awareness and timely diagnosis combined with immediate medical intervention. Consult your doctor regarding your risks and get prompt medical help if you notice any associated signs. Your health is paramount.

