Refractory celiac disease in children is an extremely rare condition where the small intestine lining does not heal, and symptoms persist despite at least 12 months of strict adherence to a gluten-free diet (GFD) and the exclusion of other possible causes for non-response (like accidental gluten exposure or other concurrent diseases). It is crucial to understand that while non-responsive celiac disease is common, true refractory celiac disease in children is exceptionally rare, affecting less than $1.9\%$ of pediatric celiac patients, and usually, it’s a disease found in adults. This diagnosis should only be made by a highly specialized pediatric gastroenterologist after a comprehensive, active investigation.
1. Defining and Identifying Refractory Celiac Disease
Before a child can be diagnosed with refractory celiac disease in children, doctors must actively rule out everything else.
The Diagnostic Process
The diagnosis is a diagnosis of exclusion, meaning the medical team systematically eliminates all other possibilities first:
- Strict GFD Confirmation: The first step is confirming $100\%$ compliance with the gluten-free diet. A specialized dietitian will review the child’s entire intake, looking for subtle sources of cross-contamination or hidden gluten. Persistent accidental gluten intake is the most common reason for persistent symptoms, not refractory celiac disease in children.
- Exclusion of Other Diseases: The doctor must actively test for other conditions that can mimic celiac symptoms and gut damage, such as Irritable Bowel Syndrome (IBS), Small Intestinal Bacterial Overgrowth (SIBO), other food intolerances (like lactose or fructose), and even other rare enteropathies (diseases of the small intestine).
- Persistent Damage: Even after all the above are ruled out, the child must still exhibit persistent small intestinal mucosal damage (villous atrophy) visible on a repeat biopsy. This is the hallmark of true refractory celiac disease in children.
The Two Types
Once diagnosed, refractory celiac disease in children is further classified into two types, based on a specific cell population in the gut lining:
- Type 1 (RCD I): This is the more common, less severe type. The cells lining the intestine (intraepithelial lymphocytes, or IELs) appear normal. This type has a relatively good prognosis and often responds to targeted therapy.
- Type 2 (RCD II): This is the most severe and aggressive type. The IELs are abnormal and clonal (monoclonal IEL proliferation). This type carries a significantly poorer prognosis and has a high risk of developing an associated T-cell lymphoma (EATL). Identifying the type is an active step that guides the entire treatment plan.
2. Active Management and Treatment Strategies
The management of true refractory celiac disease in children requires an active, multi-pronged approach and is always handled by a team in a specialized academic center.
Focusing on Nutritional Support
Because the small intestine is actively damaged and failing to absorb nutrients, nutritional status is a major concern.
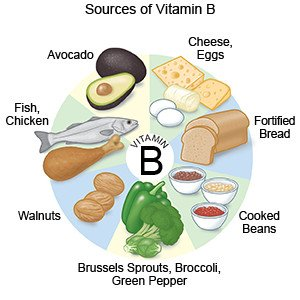
- Aggressive Supplementation: Children often require high-dose supplementation for iron, folic acid, B vitamins, and fat-soluble vitamins (A, D, E, K).
- Elemental or Enteral Feeding: In severe cases, children may need temporary total parenteral nutrition (TPN—feeding through a vein) or elemental formula feeding to allow the gut to rest and to ensure proper growth and development.
Immunosuppressive Therapy
The primary treatment for RCD is the use of medications to suppress the overly active immune response that is continuing to damage the gut lining. This is a critical step in treating refractory celiac disease in children.
- Corticosteroids: Drugs like Budesonide or Prednisone are often the first line of defense to quickly reduce gut inflammation.
- Immunosuppressants: Medications like Azathioprine or Biologics may be used, particularly for RCD Type 1, to actively control the immune system and promote mucosal healing.
- Specialized Treatments for RCD II: Due to the risk of lymphoma in Type 2, more aggressive and specialized therapies, including chemotherapy or bone marrow transplantation, may be considered in consultation with hematologists and oncologists.
3. The Importance of Specialized Care
Given its complexity and rarity, managing refractory celiac disease in children demands specialized expertise.
- Multi-Disciplinary Team: Your child needs a team that includes a highly experienced pediatric gastroenterologist, a dedicated celiac-specialist dietitian, and potentially an immunologist or oncologist.
- Continuous Monitoring: The child must be actively and frequently monitored with repeat endoscopies, biopsies, and blood tests to track immune markers and ensure mucosal healing. For RCD Type 2, surveillance for Enteropathy-Associated T-Cell Lymphoma (EATL) is an active and necessary step.
- Active Symptom Management: The team will actively manage ongoing symptoms like pain, diarrhea, and fatigue, which significantly impact the child’s quality of life and schooling.
4. Emotional and Family Support
The diagnosis of refractory celiac disease in children brings significant emotional stress to the entire family. It shatters the expectation that the GFD is a complete cure and introduces new, complex treatment regimens.
- Seek Counseling: It is beneficial for both the child and the parents to seek support from a mental health professional familiar with chronic childhood illness.
- Connect with Others: Finding support groups for parents of children with rare gastrointestinal disorders can provide valuable emotional validation and practical advice on managing the condition and the complex medications required for true refractory celiac disease in children.
- Advocacy: Parents must become active and tireless advocates for their child’s needs at school and within the healthcare system to ensure all dietary and medical needs are met.
5. Key Takeaways: Not All Non-Response is RCD
Remember the statistic: less than $1.9\%$ of pediatric celiac cases are true RCD. The vast majority of cases of non-responsive celiac disease in children are due to correctable factors.
- If your child is not improving, actively review the GFD with a celiac-experienced dietitian.
- Ask your gastroenterologist to specifically test for other common conditions like SIBO, lactose intolerance, and functional GI disorders.
- Maintain open communication with your child’s medical team throughout the intensive investigation process. Refractory celiac disease in children is a last-resort diagnosis.
Conclusion: Hope and Expertise
While the journey with refractory celiac disease in children is demanding, advancements in medical knowledge and targeted therapies offer hope. By partnering with a specialized medical team, you can actively manage this rare condition and work toward achieving mucosal healing and improving your child’s quality of life.
We strongly encourage you to seek comprehensive, evidence-based health information and specialist referrals from trusted sources. For valuable insights into managing complex health challenges, consult resources like cardiachq.com.
We want to hear from you: Has your family navigated the diagnosis of refractory celiac disease in children or another rare non-responsive GI condition? What was the most impactful treatment or support system you discovered? Share your active advice and insights below to help guide other parents facing this difficult challenge.